Prevalence and Incidence of Food Allergies in the US General Population
Ohayon MM, Duhoux S, Mouchet J, Cote ML
American College of Allergy, Asthma & Immunology (ACAAI) 2023 Annual Scientific Meeting, November 9th 13th at the Anaheim Convention Center in Anaheim, CA
Food Allergies Associations with Anxiety and Depression Disorders in the US General Population
Ohayon MM, Duhoux S, Mouchet J, Cote ML
American College of Allergy, Asthma & Immunology (ACAAI) 2023 Annual Scientific Meeting, November 9th – 13th at the Anaheim Convention Center in Anaheim, CA
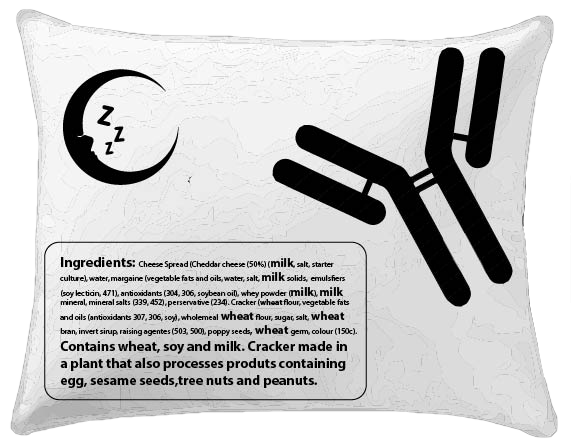
lt is increasingly accepted that one function of sleep is to support host defense. The circadian rhythm includes neuroendocrine changes that regulate human leukocyte traffic with overall immuno-supportive effects during nocturnal sleep. A normal circadian rhythm appears to enhance the efficiency of helper T cell responses. The reverse, sleep deprivation, leads to single cell alterations (including dysregulation of helper T cell function) which can result into inefficient clearance of pathogens and can cause (auto-) inflammatory diseases and auto-immunity. As we start to understand role of the sleep in (auto-) inflammatory diseases and auto-immunity, we know very little about sleep problems and the risk of developing allergic/immunological conditions. Nevertheless, there are hints of at least a moderating effect of sleep coming from 2 studies:
An allergic response can, not only be conditioned to a specific cue, but also be triggered by merely reencountering the environmental context in which an allergen was previously encountered. However, the allergic response to the reencountering experience only occurs with normal sleep. lt does not occur when subjects are forced to stay awake. This shows the critical role of sleep in the formation of a memory for allergic responses.
ln mice, poor sleep quality contributes to a more severe form of asthma: the progression of allergen-induced eosinophilic lung inflammation to a corticosteroid-refractory neutrophilic manifestation.
Sleep disturbance is associated with a decrease in regulatory T cells. ln lnfants, the decrease in regulatory T cells is shown to be linked to hyper-responsiveness in food allergy.
This symposium aimed to explore the fields of sleep, immunology and allergies with experts from around the world and discuss the latest advancements in these respective fields. Finally, our objective was to have a better understanding of the inter-relations between sleep, immunology and allergies.